Drug addict的問題,我們搜遍了碩博士論文和台灣出版的書籍,推薦Woods, Ww寫的 Walking a Tightrope: How the Disease of Addiction Affects Everything!!!: A Practical Guide on How to Stay Clean in Spite of Ours 和Bush, Nicholas的 One by One: A Memoir of Love and Loss in the Shadows of Opioid America都 可以從中找到所需的評價。
另外網站Helping a Friend With an Addiction - Health Encyclopedia也說明:Addiction means losing control over your drug use. Or losing insight into knowing how or when to stop. Addiction begins with alcohol or drug abuse. Drugs and ...
這兩本書分別來自 和所出版 。
臺北醫學大學 國際醫學研究博士學位學程 白其卉、DUONG VAN TUYEN所指導 NGUYEN HOANG MINH的 Mental Health, Health-related Quality of Life and Behaviors among Outpatients during the COVID-19 Pandemic: A Multiple Hospitals and Health Centers Study in Vietnam (2021),提出Drug addict關鍵因素是什麼,來自於COVID-19、health-related quality of life、health behaviors、health literacy、lockdown、underlying health conditions、fear、anxiety、depression、outpatients。
而第二篇論文慈濟大學 人類發展與心理學系碩士班臨床心理學組 陳紹祖所指導 葉育修的 酒精使用障礙症合併憂鬱情緒患者接受認知行為治療之個案研究 (2021),提出因為有 酒精使用障礙症、憂鬱症、認知行為治療、述情障礙、家庭作業完成的重點而找出了 Drug addict的解答。
最後網站7 Tips for Helping Someone with an Addiction | TriHealth則補充:The challenge with addiction is that the addict is not the only one impacted by this disease. Here are seven tips you can reference to support an addicted ...
Walking a Tightrope: How the Disease of Addiction Affects Everything!!!: A Practical Guide on How to Stay Clean in Spite of Ours

為了解決Drug addict 的問題,作者Woods, Ww 這樣論述:
This is a book about ongoing recovery from drug and alcohol addiction. It is a collection of approaches that I have used in the past thirty years to build and maintain a semi normal and sane methodology for clean living. Recovery is not for the faint of heart, as the disease affects every aspect
of our lives, continues to live inside us even after we establish abstinence and is just waiting for an opportunity to weasel its way back into our lives and fulfill its quest: Jails, Institutions and Death. The writing is a collection of stories, personal experiences and real world examples of what
it is like to be a recovering addict. It is meant to be funny, inspirational and maybe even tragic in some respects. The intent is to be as factual as possible without violating any of the participants anonymity. My personal hope is that this provides someone out there with an opportunity and hope
of living a regular spiritually based life. Life is a spiritual journey and we need to work for that!
Drug addict進入發燒排行的影片
▶ 點這裡訂閱我的頻道 ❤️ http://www.youtube.com/可恩keEn
▶ 喜歡我的影片,記得幫我【分享】和【按讚】喲~
▶ Follow 可恩:
FB: http://www.facebook.com/katemeowwww
IG: http://www.instagram.com/fluffywingss
▶ 任何合作邀約,請直接聯繫:
[email protected]
[email protected]
Mental Health, Health-related Quality of Life and Behaviors among Outpatients during the COVID-19 Pandemic: A Multiple Hospitals and Health Centers Study in Vietnam
為了解決Drug addict 的問題,作者NGUYEN HOANG MINH 這樣論述:
BackgroundGlobally, the coronavirus disease (COVID-19) pandemic has been placing unprecedented challenges and burdens on various aspects of life, such as economics, culture, politics, education, and healthcare. The uncertainty of COVID-19 increases concerns and fear in the communities, especially i
n those with symptoms like COVID-19 (S-LikeCV19). Additionally, many countries have implemented preventive measures (e.g., lockdown, home confinement, social distancing), leading to considerable changes in peoples’ lives, such as working and learning from home, unemployment, lack of physical connect
ion, and food insecurity. Besides, it is reported that people with underlying health conditions (UHC) and infected with COVID-19 have a higher risk of serious symptoms and complications. Therefore, COVID-19-related factors (e.g., fear, lockdown, S-LikeCV19) and UHC may influence peoples’ psychologic
al health and health behaviors, further lowering their health-related quality of life (HRQoL). Furthermore, people who need health services encountered many challenges during the pandemic, such as difficulties in accessibility, examination and treatment delays, and concerns about COVID-19 infection.
From a public health perspective, it is crucial to understand the impacts of COVID-19-related factors and explore protective factors that can improve lifestyles, psychological health, and HRQoL in outpatients. In addition, due to unavailable specific treatments, non-pharmaceutical interventions (e.g
., adherence to preventive measures, health knowledge improvement, healthy lifestyles) are highly recommended to mitigate the consequences of the COVID-19 pandemic.Therefore, this study was conducted on outpatients during the initial stage of the COVID-19 pandemic for the following purposes:(1) To e
xplore the impacts of UHC, S-LikeCV19, and lockdown on anxiety and depressive symptoms; and examine the modification effects of health behaviors (e.g., eating behaviors, physical activity, smoking, drinking) and preventive behaviors.(2) To explore impacts of UHC, S-LikeCV19, lockdown, and fear of CO
VID-19 (F-CV19) on HRQoL; and examine the modification effects of health literacy, eHealth literacy (eHEALS), digital healthy diet literacy (DDL).(3) To explore impacts of UHC, S-LikeCV19, lockdown, and fear of COVID-19 (F-CV19) on changes in eating behaviors and physical activity; and examine the m
odification effects of eHEALS, DDL.MethodsA cross-sectional study was conducted from 14th February to 31st May 2020 in 18 hospitals and health centers in Vietnam. Data were obtained from 8291 outpatients, including socio-demographic characteristics, UHC, S-LikeCV19, F-CV19, health-related behaviors
(smoking, drinking, eating behaviors, and physical activity), preventive behaviors, eHEALS, DDL, depression (measured by 9-item Patient Health Questionnaire), anxiety (measured by 7-item Generalized Anxiety Disorders), and HRQoL (measured by 36-item Short Form Survey). In addition, multiple linear a
nd logistic regression; and interaction models were performed to explore potential associations.ResultsThe prevalence of anxiety and depression was 12.5% and 22.3%, respectively. Patients with UHC had 3.44 times higher anxiety likelihood and 2.71 times higher depression likelihood, while patients wi
th S-LikeCV19 had 3.31 times higher anxiety likelihood and 3.15 times higher depression likelihood than their counterparts. Similarly, patients under lockdown were 2.39 and 2.89 times more likely to have anxiety and depression than those without lockdown, respectively. Interaction models indicated h
igh compliance with preventive behaviors, unchanged/more physical activity, and unchanged/healthier eating behaviors significantly attenuated the associations of UHC, S-LikeCV19, and lockdown with anxiety and depressive symptoms. In addition, unchanged/more alcohol drinking significantly attenuated
the association between UHC and anxiety. Furthermore, the association between S-LikeCV19 and depression was attenuated by higher health literacy scores in outpatients during the pandemic.This study showed that only fear of COVID-19 was negatively associated with HRQoL (B, -0.79; 95% CI, -0.88 to -0.
70; p < 0.001). Interaction models suggested that the inverse association between F-CV19 and HRQoL was mitigated by higher eHEALS scores or higher DDL scores.Patients with UHC, or with S-LikeCV19, or under lockdown had 54%, 52%, and 62% lower likelihoods of unchanged/healthier eating behaviors, and
21%, 58%, and 22% lower likelihoods of unchanged/more physical activity. Interaction models indicated that the association between lockdown and eating behaviors was significantly attenuated by higher DDL scores. Meanwhile, the association between lockdown and physical activity was significantly miti
gated by higher eHEALS scores. There was no statistically significant interaction of UHC and S-LikeCV19 with DDL and eHEALS on changes in health behavior outcomes.Conclusions:During the pandemic, patients under lockdown period, or with UHC, or S-LikeCV19 were more likely to have anxiety and depressi
ve symptoms; and less likely to have unchanged/healthier eating behaviors and unchanged/more physical activity. In addition, patients with higher F-CV19 were more likely to have poorer HRQoL.High adherence to preventive behaviors, physical activity, and healthy eating behaviors could mitigate the ne
gative impacts of UHC, S-LikeCV19, and lockdown on anxiety and depression. In addition, higher health literacy could mitigate the impact of S-LikeCV19 on depression during the pandemic. Besides, alcohol drinking was found to lower the impact of UHC on anxiety.Moreover, better eHEALS and DDL could mi
tigate the adverse impacts of F-CV19 on HRQoL. Higher eHEALS could help to alleviate the impact of lockdown on physical activity, while higher DDL could mitigate the impact of lockdown on eating behaviors.Our findings provide timely and reliable evidence for appropriate strategies to enhance healthy
lifestyles, preventive behaviors, eHEALS, and DDL, thereby preventing outpatients from psychological disorders and improving their HRQoL during the pandemic.
One by One: A Memoir of Love and Loss in the Shadows of Opioid America
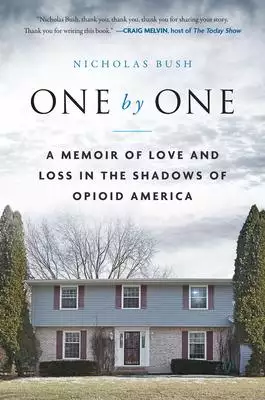
為了解決Drug addict 的問題,作者Bush, Nicholas 這樣論述:
Nicholas Bush is a reformed drug addict who works with addicts and criminals in halfway houses and prisons to help them turn their lives around. He began combatting his own addiction after losing a sister and a brother to drug overdoses. Bush has written articles related to opioid addiction for USA
Today, the New York Post, PBS, and the Johns Hopkins Medical Journal, and been featured on The Today Show. He is from Green Bay, Wisconsin, and lived for many years in Kansas City, Missouri, but currently resides in Mendocino, California, with his wife and young daughters.
酒精使用障礙症合併憂鬱情緒患者接受認知行為治療之個案研究
為了解決Drug addict 的問題,作者葉育修 這樣論述:
摘要:本研究以個案報告記錄三位「酒精使用障礙症」(Alcohol use disorder, AUD)合併「憂鬱症」(Major depressive disorder, MDD)患者接受「認知行為治療」(Cognitive Behavior Therapy, CBT) 的歷程。本研究分為四個階段,第一階段於身心科門診或病房收案;第二階段在病患充分知情同意後納入研究,並施行心理測驗評估病患的認知功能可接受「認知行為治療」(Cognitive Behavior Therapy, CBT)。第三階段,病患會接受12次CBT治療,並在最後一次治療時,接受心理測驗。第四階段在結案後一個月再進行追蹤訪
談與評估CBT療效。研究結果發現,個案在接受認知行為治療時,有助於療效因子分為內在因素與外在因素。內在因素包括:病患能修改失功能的信念與負面的自動化思考,提升回家作業遵從性,並且在渴求時採取有效因應策略。外在因素為正向積極的社交支持力量。無助於療效的因子,包括:在治療時,病患不願意揭露實際飲酒情況與憂鬱情緒,無法與治療師建立合作同盟的治療關係,回家作業遵從性不佳與欠缺社群支持。此外,本研究建議酒精使用障礙症合併有憂鬱情緒與述情障礙特質者,認知行為治療重點應著重於教導病患辨識在高風險情境中促進飲酒的信念,並且使用行為活化技巧對應渴求與憂鬱情緒。最後,本研究結果為相關領域提供更近一步量化研究基礎,
並且提供該族群接受更有效評估與臨床介入方式。
想知道Drug addict更多一定要看下面主題
Drug addict的網路口碑排行榜
-
-
#2.Drug Addiction - OpenDOSM - Department of Statistics Malaysia
Every year, DOSM works with the National Anti-Drugs Agency (NADA) to release statistics on drug addiction as part of the annual crime statistics release. 於 open.dosm.gov.my -
#3.Helping a Friend With an Addiction - Health Encyclopedia
Addiction means losing control over your drug use. Or losing insight into knowing how or when to stop. Addiction begins with alcohol or drug abuse. Drugs and ... 於 www.urmc.rochester.edu -
#4.7 Tips for Helping Someone with an Addiction | TriHealth
The challenge with addiction is that the addict is not the only one impacted by this disease. Here are seven tips you can reference to support an addicted ... 於 www.trihealth.com -
#5.Chasing the Dragon: The Life of an Opiate Addict - FBI
In an effort to combat the growing epidemic of prescription drug and heroin abuse, the FBI and DEA have released "Chasing the Dragon: The Life of an Opiate ... 於 www.fbi.gov -
#6.Follow-up of Former Drug Addict and Alcoholic Beneficiaries
The Social Security Act Amendments of 1972 ( P.L. 92-603) were the first provisions to specifically address drug addicts and alcoholics (DA&As) in the DI or SSI ... 於 www.ssa.gov -
#7.Genes matter in addiction - American Psychological Association
At least half of a person's susceptibility to drug addiction can be linked to genetic factors. Presenters at an April 8 congressional ... 於 www.apa.org -
#8.Addiction: Definition, symptoms, withdrawal, and treatment
Addiction is a condition in which a person is unable to stop using a substance or engaging in a behavior. Read on to learn more. 於 www.medicalnewstoday.com -
#9.My Name is Aidan and I am a drug addict. This is my story.
At age 15, I was smoking marijuana any moment I could and soon found out that everyone around me was drinking alcohol so I thought I would try it. I thought “my ... 於 cedarscobblehill.com -
#10.Helping an Adult Family Member or Friend with a Drug or ...
Describe your family member's substance use pattern to see whether the professional would deem it a problem. Provide details such as: type of alcohol or other ... 於 drugfree.org -
#11.Signs of Addiction | Drugs, Alcohol, & Prescription Drugs
According to the National Council on Alcoholism and Drug Dependence, withdrawal symptoms may include but are not limited to: Shakiness, trembling, and jumpiness ... 於 www.advancedrecoverysystems.com -
#12.Drug Use and Addiction - MedlinePlus
There are different types of treatment for drug abuse but the best is to prevent it. Understand more about substance abuse. 於 medlineplus.gov -
#13.Alcoholism and Drug Addiction - Termedia
Alcoholism and Drug Addiction/Alkoholizm i Narkomania is an official journal of the Institute of Psychiatry and Neurology in Warsaw. 於 www.termedia.pl -
#14.Substance Abuse under the ADA
An employer may not discriminate against a person who has a history of drug addiction but who is not currently using drugs and who has been rehabilitated. An ... 於 www.usccr.gov -
#15.The Effects of Drug Addiction on the Brain and Body
Substance abuse has many consequences. Learn about the short and long-term effects of drug addiction. Discover treatment options for common ... 於 www.verywellhealth.com -
#16.Recognizing the Warning Signs of Drug Addiction: What You ...
1. Physical Evidence: Drug Paraphernalia · 2. Stashes of the Drug · 3. Increasing Risk-Taking Behaviour · 4. Altered Physical Appearance · 5. The Inability to Quit ... 於 intercoast.edu -
#17.Was Sherlock Holmes an Addict? - Banyan Treatment Center
What was he addicted to? Visit us here to learn about Arthur Conan Doyle's beloved detective and his struggles with drug abuse. 於 www.banyantreatmentcenter.com -
#18.Drug addiction vs. drug abuse - The Diamond Rehab Thailand
On the other hand, drug abuse is the act of using prescription medications in ways other than intended or using drugs to achieve euphoria or “ ... 於 diamondrehabthailand.com -
#19.What Causes Drug Addiction? | Casa Palmera
Addictive substances such as nicotine, alcohol, opioid medications, and marijuana are considered drugs just as much as heroin, cocaine, or ... 於 casapalmera.com -
#20.Addiction | Health Navigator NZ
Common addictions include: alcohol; cigarettes (tobacco); P (meth), cannabis and other illegal drugs; prescription medicines; gambling; gaming ... 於 www.healthnavigator.org.nz -
#21.Does addiction last a lifetime? - Harvard Health
Can a person who was addicted to drugs or alcohol in their teens safely have a glass of wine with dinner in their middle age? 於 www.health.harvard.edu -
#22.10 Signs of Drug Abuse, Use, or Addiction - Cirque Lodge
We offer signs of drug use, abuse, addiction indications that you can look for if you think that you. 於 www.cirquelodge.com -
#23.Dealing With Addiction (for Teens) - Nemours KidsHealth
Addiction begins as abuse, or using a substance like marijuana or cocaine. You can abuse a drug (or alcohol) without having an addiction. For example, just ... 於 kidshealth.org -
#24.What Is Drug Addiction? - Pinnacle Treatment Centers
Drug Addiction Facts & Stats. Most people who suffer with substance abuse disorder (SUD) tend to hide their condition and prefer not to be vocal ... 於 pinnacletreatment.com -
#25.Drug Addiction and Federal Disability Rights Laws Fact Sheet
sleeping, walking, standing, lifting, bending, speaking, breathing, learning, reading, concentrating, thinking, communicating, and working. 於 www.hhs.gov -
#26.Does Addiction Run In Families? What Statistics Reveal
Why do some people become addicted to drugs and alcohol while others don't? Is it all due to our environment, or do genetics play a role in ... 於 www.orlandorecovery.com -
#27.Addiction - Wikipedia
Similar to other behavioral addictions, CBD can be linked to mood disorders, substance use disorders, eating disorders, and other disorders involving a lack of ... 於 en.wikipedia.org -
#28.Chapter 8 - Drug Abuse or Drug Addiction | USCIS
A. Drug Abuse or Drug Addiction Applicants who are found to be drug abusers or addicts are inadmissible.&n. 於 www.uscis.gov -
#29.Drug Abuse and Addiction - HelpGuide.org
Do you or someone you love have a problem with substance abuse? Explore the warning signs and how to get the best help. 於 www.helpguide.org -
#30.Lil Pump - Drug Addicts [Official Music Video] - YouTube
Watch the official music video for Drug Addicts by Lil Pump from the album Harverd Dropout. Subscribe to the channel: ... 於 www.youtube.com -
#31.What is the Definition of Addiction?
... titles of predecessor organizations: alcoholism, alcohol and other drug dependencies, addictionology, and, finally, addiction medicine. 於 www.asam.org -
#32.Drug addict Definition & Meaning - Dictionary.com
Drug addict definition, a person who is addicted to a chemical substance, especially a narcotic. See more. 於 www.dictionary.com -
#33.10 Things to Do When You're Married to an Addict
Drugs and alcohol are their priority, not you and your family. You may have tried everything you can think of to help your addicted spouse. It's ... 於 www.recoveryranchpa.com -
#34.Reporting drug dependence - WA Health
On receiving a report the Chief Executive Officer may decide to include the name of the person on the drugs of addiction record as a Drug Dependent person. 於 www.health.wa.gov.au -
#35.Why Do People Get Addicted to Drugs? | Turnbridge
Drug addiction can happen to anyone. Still, the question remains, why do some people get addicted to drugs, while others do not? Learn the causes of ... 於 www.turnbridge.com -
#36.Drug addiction (substance use disorder) - Mayo Clinic
Substances such as alcohol, marijuana and nicotine also are considered drugs. When you're addicted, you may continue using the drug despite the harm it causes. 於 www.mayoclinic.org -
#37.What is Drug Addiction | Origins Behavioral Healthcare
Learn about drug addiction, warning signs, commonly used drugs, and the best treatment for this complex brain disease. 於 www.originsrecovery.com -
#38.Loving a Drug Addict: Do People With Addiction Love Back?
Alcohol and other drugs affect all aspects of life, including relationships, meaning people must learn how to adjust and respond to the ... 於 www.floridarehab.com -
#39.Behavior of Drug Addict in Active Addiction | La Hacienda
When most people think of addiction, they think of drugs or alcohol. However, addiction can be much more complicated. 於 www.lahacienda.com -
#40.Dopamine in Drug Abuse and Addiction: Results of Imaging ...
Imaging studies have provided new insights on the role of dopamine (DA) in drug abuse and addiction in the human brain. These studies have shown that the ... 於 jamanetwork.com -
#41.Knowing When and How to Leave a Drug Addict
Why Do People Stay in a Romantic Relationship With an Addict? Reasons Why People Should Leave Relationships With Addicts. Abuse; You Enable the ... 於 www.phoenixrisingrecovery.com -
#42.Signs of Drug Use & Addiction: How To Tell if Someone Is On ...
Knowing these signs can help to identify whether a loved one may be using drugs or addicted to a substance of abuse and risking harmful ... 於 americanaddictioncenters.org -
#43.Ways of Helping Someone with Drug or Alcohol Addiction
Learn how to get drug addiction help or how to help a drug addict quit using. Read about substance abuse and ways of helping someone who has has abused ... 於 drugabuse.com -
#44.How to help someone who is misusing drugs or alcohol
Supporting a friend or family member who's struggling with drug or alcohol misuse is not easy. These tips and resources may help. 於 www.healthdirect.gov.au -
#45.Understanding Drug Use and Addiction DrugFacts
Provides an overview of drug use and addiction, including what happens in the brain during drug use, why some people become addicted while ... 於 nida.nih.gov -
#46.Addiction | Health Effects | Marijuana | CDC
... Another study estimated that people who use cannabis have about a 10% likelihood of becoming addicted. 2 ; The risk of developing marijuana use disorder ... 於 www.cdc.gov -
#47.79 Synonyms & Antonyms of ADDICT - Merriam-Webster
a person who regularly uses drugs especially illegally an inspiring story about addicts who seek help and manage to kick their habit. 於 www.merriam-webster.com -
#48.Characteristics and Symptoms of Drug Addictions
The emotional and psychological aspects of drug addiction are every bit as powerful and life-altering as the physical effects of substance dependence. 於 www.altamirarecovery.com -
#49.What is a High Functioning Addict? - Laguna Treatment Hospital
The notion of a “functional drug addict” is actually a contradiction of terms. When anyone uses the term addiction or addict, ... 於 lagunatreatment.com -
#50.How Drug Addiction Affects The Entire Family - Peace Valley
Find out how addiction affects the entire family in this post. The impact of drug and alcohol addiction ripples far beyond the addict. 於 www.peacevalleyrecovery.com -
#51.Drug use and addiction care - Government.nl
Drug use can have an adverse effect on users and on public health. The government seeks to prevent people using drugs. If people nonetheless become addicted ... 於 www.government.nl -
#52.When Does Drug Use Become an Addiction? - Verywell Mind
Drug addiction has been characterized as a complex and chronic brain disease that can cause compulsive drug-seeking in spite of negative ... 於 www.verywellmind.com -
#53.Five Psychological Effects of Drug Addiction | RACNJ
Read on to find out more about the emotional effects of substance use disorders. Drug Abuse Rewires Your Brain. One of the most profound changes ... 於 www.racnj.com -
#54.Office of Addiction Services and Supports | Office of Addiction ...
Join the Addiction Services Workforce. OASAS oversees the credentialing of substance use counselors and prevention practitioners in New York. 於 oasas.ny.gov -
#55.Addiction | Psychology Today
Substance use and gambling disorders not only engage the same brain mechanisms, they respond to many of the same treatment approaches. Substance use and ... 於 www.psychologytoday.com -
#56.Drug Addiction Consequences - Summit BHC
There are numerous drug addiction consequences. They can affect us physically, mentally, socially and spiritually, to varying degrees. 於 summitbhc.com -
#57.Study: Public Feels More Negative Toward People With Drug ...
People are significantly more likely to have negative attitudes toward those suffering from drug addiction than those with mental illness, ... 於 publichealth.jhu.edu -
#58.High Functioning Addict | Sierra by the Sea
Experiencing cravings to have more of a drug; Behaving in uncharacteristic ways when under the influence of drugs or alcohol; Denying the existence of a problem ... 於 www.sierrabythesea.com -
#59.Neuropathology of Drug Addictions and Substance Misuse
Neuropathology of Drug Addictions and Substance Misuse, Volume One: Foundations of Understanding, Tobacco, Alcohol, Cannabinoids, Opioids and Emerging ... 於 www.sciencedirect.com -
#60.Substance Use Disorder (SUD): Symptoms & Treatment
Substance use disorder (SUD) is a mental health condition in which a person has a problematic pattern of substance use that causes distress ... 於 my.clevelandclinic.org -
#61.14 Synonyms & Antonyms for DRUG ADDICT - Thesaurus.com
Find 14 ways to say DRUG ADDICT, along with antonyms, related words, and example sentences at Thesaurus.com, the world's most trusted free thesaurus. 於 www.thesaurus.com -
#62.Drug addiction - Counselling Directory
For some people, drug abuse spirals into addiction. When this happens, getting and using drugs becomes an all-consuming activity that can affect ... 於 www.counselling-directory.org.uk -
#63.NCDAS: Substance Abuse and Addiction Statistics [2023]
The National Center for Drug Abuse Statistics has the latest facts & statistics on substance abuse, including alcoholism & opioid addiction. 於 drugabusestatistics.org -
#64.Understanding Drug Abuse and Addiction
Many people do not understand why individuals become addicted to drugs or how drugs change the brain to foster compulsive drug abuse. 於 dmh.lacounty.gov -
#65.The Trauma of Children of People With Addiction | Psych Central
Growing up with a parent who has alcohol or substance use disorder can lead to negative effects on your mental health and more. However, there's hope. 於 psychcentral.com -
#66.Drug Addiction Images - Free Download on Freepik
Find & Download Free Graphic Resources for Drug Addiction. 90000+ Vectors, Stock Photos & PSD files. ✓ Free for commercial use ✓ High Quality Images. 於 www.freepik.com -
#67.Is Drug Addiction a Mental Illness?
According to the National Institute on Drug Abuse (NIDA) drug addiction is classified as a mental illness because addiction changes the brain in fundamental ... 於 drugfreeclermont.org -
#68.How To Identify Drug Addiction Symptoms in Your Loved One
Heroin and opioid addictions are the most prevalent in America, and deaths related to overdoses from these addictive substances have increased over 300% since ... 於 sbtreatment.com -
#69.Drug addict definition and meaning | Collins English Dictionary
Drug addict definition: A drug addict is someone who is addicted to illegal drugs. | Meaning, pronunciation, translations and examples. 於 www.collinsdictionary.com -
#70.Turning Point addiction treatment, education and research ...
Turning Point is an Australian addiction research and education centre that provides treatment for people adversely affected by alcohol, drugs and gambling. 於 www.turningpoint.org.au -
#71.How Should We Describe A Person With An Addiction? - NPR
Journalists should quit calling a person who uses drugs an "addict," according to The Associated Press Stylebook. This follows a trend ... 於 www.npr.org -
#72.How to help a friend with drug addiction - ReachOut Australia
If you're worried about a friend who you think may be addicted to drugs, it's good to know what to look for. The good news is that you can help them more ... 於 au.reachout.com -
#73.Am I a Drug Addict? (11 Signs of Addiction)
Assessing whether or not you are suffering from substance abuse or addiction problem is no easy task. 於 oxfordtreatment.com -
#74.Drug Abuse and Addiction Research at Johns Hopkins ...
IBBS researchers are studying how chronic drug use causes lasting changes in the brain that can lead to addiction. Their findings may aid in the development ... 於 www.hopkinsmedicine.org -
#75.Cocaine Abuse & Addiction - NYC.gov
What is Cocaine? Cocaine is a powerfully addictive stimulant that directly affects the brain. Cocaine has been labeled the drug of the 1980s and '90s, because ... 於 www.nyc.gov -
#76.The evolutionary origins and significance of drug addiction
Gaining an understanding of the implications of ancient psychotropic substance use in altering mammalian brains will assist in assessing the ... 於 harmreductionjournal.biomedcentral.com -
#77.5 ways to prevent drug addiction - Fairwinds Treatment Center
People become addicted to drugs for many reasons. Some of their motives include trying to overcome another mental disorder, like depression, ... 於 fairwindstreatment.com -
#78.How To Let Go of a Drug Addict - Family First Intervention
These principles, along with the family's recovery, can help start the process of detaching and letting go of the loved one's addiction. Who ... 於 family-intervention.com -
#79.EMCDDA home page | www.emcdda.europa.eu
Explore the latest findings from the largest European project in the science of wastewater analysis, with over 104 European cities from 21 countries. Explore ... 於 www.emcdda.europa.eu -
#80.Addiction Treatment Medications
Medication can help those recovering from addiction stay sober. Addiction medications can reduce both cravings and long-term withdrawal ... 於 www.addictioncenter.com -
#81.532875 Drug Addict Images, Stock Photos & Vectors
Find Drug Addict stock images in HD and millions of other royalty-free stock photos, illustrations and vectors in the Shutterstock collection. 於 www.shutterstock.com -
#82.How to help a friend | FRANK
If you think your friend has a problem with drugs, get advice and support on how you can help them. Find out more online. 於 www.talktofrank.com -
#83.Drug and alcohol addiction - useful contacts - Mind
Alcohol support organisations · Alcoholics Anonymous (AA) · Alcohol Change UK · FRANK · London Friend · Turning Point · We Are With You. 於 www.mind.org.uk -
#84.How Does Addiction Affect Your Life? - MyHealth Alberta
Alcohol, drugs, tobacco, and gambling can affect many areas in your life. It can help to look closely at these areas to see what the effects have been. 於 myhealth.alberta.ca -
#85.Drug Abuse & Addiction: Effects on Brain, Risk Factors, Signs
When you're addicted to drugs, you can't resist the urge to use them, no matter how much harm the drugs may cause. The earlier you get treatment ... 於 www.webmd.com -
#86.To end the drug crisis, bring addiction out of the shadows
Shame and stigma fuel addiction and prevent treatment, argues Nora Volkow, MD, director of the National Institute on Drug Abuse. 於 www.aamc.org -
#87.What Is a Substance Use Disorder? - Psychiatry.org
Addiction is a complex condition, a brain disease that is manifested by compulsive substance use despite harmful consequence. Learn more at psychiatry.org. 於 www.psychiatry.org -
#88.Drug addiction - World Health Organization (WHO)
Substance dependence/addiction, in- volving both a common brain reward mechanism and longer-lasting molecular and cellular chang- es, is a preventable chronic, ... 於 apps.who.int -
#89.Drug addiction | Drug abuse signs and symptoms
Drug addiction, or substance use disorder, is characterised by the compulsive consumption of drugs despite their danger. 於 www.ukat.co.uk -
#90.Children Living with Parents Who Have a Substance Use ...
This report uses data from the 2009 to 2014 National Surveys on Drug Use and Health (NSDUHs) to determine the number of children aged 17 or ... 於 www.samhsa.gov -
#91.Living with an Addict: What to Know and How to Cope
In order to live with a loved one who has an addiction or is in recovery, it's important to understand the disease. 於 www.healthline.com -
#92.How To Confront a Drug Addict - The Recovery Village
For example, drug addicts will often lie and steal to get more drugs. They will also try to manipulate situations to facilitate their addiction. 於 www.therecoveryvillage.com -
#93.World Drug Report 2019: 35 million people worldwide suffer ...
Vienna, 26 June 2019 - Improved research and more precise data have revealed that the adverse health consequences of drug use are more severe and widespread ... 於 www.unodc.org -
#94.Addiction: what is it? - NHS
Addiction is most commonly associated with gambling, drugs, alcohol and smoking, but it's possible to be addicted to just about anything, including: work – some ... 於 www.nhs.uk -
#95.The Physical & Mental Effects of Drug Abuse
Clinically known as substance use disorder, drug abuse or addiction is caused by the habitual taking of addictive substances. Drugs include alcohol, marijuana, ... 於 www.gatewayfoundation.org -
#96.How to Help a Drug Addict - wikiHow
What if you want to help someone who is addicted to drugs, but you don't know how? There are many misconceptions about how to help a person who has an ... 於 www.wikihow.com -
#97.Warning Signs of Drug Abuse - TN.gov
Use of recreational drugs, over the counter medications or prescription drugs can lead to substance use issues. It can frequently lead to problems at work, ... 於 www.tn.gov -
#98.What to do if your adult child is an addict - The Liberty Ranch
Are you concerned that your adult child has a drug or alcohol addiction? This comprehensive guide will help you recognize the signs and ... 於 thelibertyranch.com